Blog
Value-Based Purchasing and the Role of Home Care Software, Our Ultimate Guide

What’s the best way to pay those who deliver home care services? The issue remains elusive when it comes to firm answers. It also remains a point of seemingly endless debate and consternation, which isn’t surprising when so much money, deep implications, and sensitivities collide in one discussion.
But there’s no longer denying what’s happening in countries like the United States. As healthcare costs spiral into the stratosphere — driven by a tsunami of baby boomers who are not only living longer but doing so amid escalating rates of chronic diseases — governments and healthcare organizations must grapple with how to manage the bottom line while providing top-notch care.
The overall picture is jarring: the U.S. Centers for Medicare and Medicaid Services predicts that health spending will grow at an average annual rate of 5.4 percent for 2019-28 and
to reach $6.2 trillion by 2028.
“The transition to a value-based care delivery model is projected to benefit patients, providers, payers, vendors, and society as a whole… While it gains a foothold on the national stage, providers remain optimistic about the financial and clinical outcomes value-based care could yield in the coming years, and Home Health Care News (HHCN) set out to explore the drivers behind that sentiment.” – Andrew Dolan, Editor Home Health Care News
Value-Based Purchasing (VBP)
What is value-based purchasing?
“Linking provider payments to improved performance by health care providers. This form of payment holds health care providers accountable for both the cost and quality of care they provide. It attempts to reduce inappropriate care and to identify and reward the best-performing providers.”
Fortunately, with the rise of technology, we’ve reached the age of efficiency even when it comes to healthcare and the world of home care within it.
” The original HHVBP Model resulted in an average 4.6 percent improvement in HHAs’ total performance scores (TPS) and an average annual savings of $141 million to Medicare without evidence of adverse risks.”
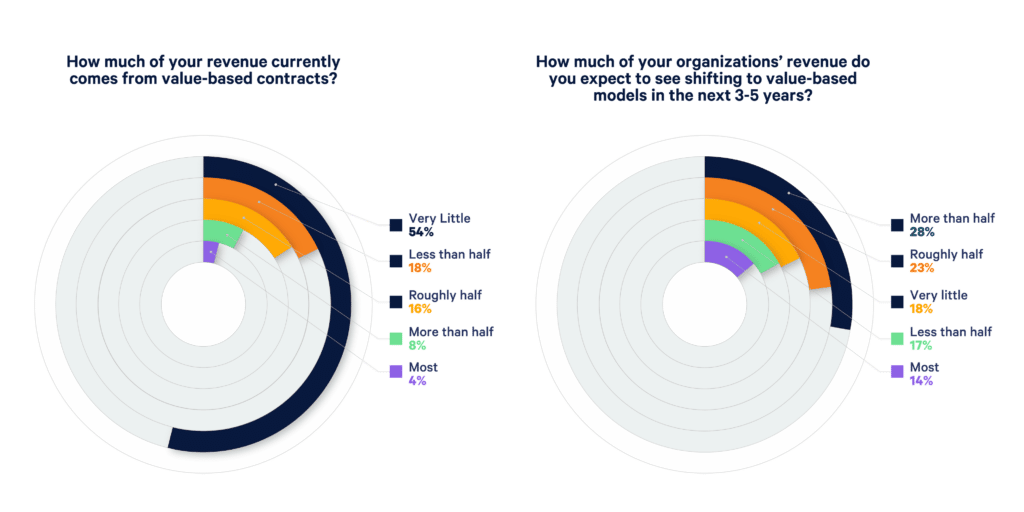
Health policy discussions have given way to actions. According to a survey on Value-based pay by Home Health Care News (HHCN) and AlayaCare, 54% of home care providers say that currently very little of their revenue comes from value-based contracts. However, this number drastically shifts with 51% of respondents identifying that roughly half or more of their revenue will come from value-based pay in the next 3-5 years.
Organizations in the business of delivering care that is prepared for this shift will be the same ones that thrive in a new marketplace.
While the U.S. routinely ranks first in the world in healthcare spending, indicators show that health performance in the country lags well behind other comparable nations. So, we spend the most money per capita, but our collective health does not improve over others who spend less.
Clearly, something needed to change, which gave rise to the value-over-volume idea. Today, the future is here and value-based purchasing (VBP) is here to stay. VBP programs are aligning payment with quality care; therefore, organizations will need an effective quality plan that will show measurable improvement in patient outcomes to remain sustainable and thrive.
In VBP, payment correlates to each provider achieving a suite of defined, measured goals tied to such aspects as quality of care, patient experience, patient outcomes, and resources used. Through this model, we can overcome the negative issues associated with FFS.
Some of the potential benefits inherent to VBP include:
- Optimized outcomes
- Improved delivery of care
- More efficient, higher-value care
- Greater accountability among providers
- Greater collaboration and connectivity among providers involved with any one patient
- Reduced risk of fragmented care
- Opportunities for great data analysis, both clinical and financial
“The HHVP is estimated to save Medicare $378 million in reduced spending for inpatient hospitalization and SNF stays by 2022.”
According to the VBP Survey by HHCN and AlayaCare, 63% of care providers see the biggest benefit of Value-based care to be better client outcomes.

The success of the home health value-based purchasing pilot program is the reason that CMS is embarking on a national expansion of the reimbursement model. To succeed, organizations will need to create a plan.
Key dates to know:
- 2022 – pre-implementation year
- 2023 – first performance year with data used to determine the first VBP payment
- 2025 – first payment year with adjustments
The value of preparation will affect reimbursement, as those agencies who perform above average will share in the savings up to a 5% maximum and those who perform below average will lose reimbursement up to 5% compared to similar sized agencies across the country.
Take advantage of this pre-implementation year and prepare now. Download our VBP e-guide.
Leverage Technology to Greet VBP
If we hone in on home care, it is abundantly clear that technology will be needed to manage the incoming world of VBP. Agencies will need the right software to clearly track how patients and clients are doing and demonstrate the value of the care delivered. Those who run referring sources like hospitals and skilled nursing facilities will want to know this information now more than ever.
The need for a seamless flow of data and analytics will be off-the-charts important. Such information will show and indeed prove, just how much both medical and non-medical services boost the quality of life and outcomes for clients. Any paper-based reporting will be very problematic in the VBP environment.
“Technology plays a leading role in the shift toward value and outcomes-focused care. Agencies need the ability to benchmark and report on patient outcomes and care quality, which necessitates the need to capture more health data and more robust analytics. AlayaCare not only offers the means to first collect and report on the data for payers, MCOs, and referral sources, but it also allows care providers to use AI tools to predict adverse events and see trends to intervene, prior to seeing any failing VBP metrics.” – Patrick Charbonneau, SVP, Product AlayaCare
Home health agencies must put their Quality Assessment/Performance Improvement (QAPI) programs at the forefront and should be ready for an assortment of quality
performance metrics that payers build into their payment system. These will include metrics related to health system usage, like the percentage of clients admitted to the hospital in the past 90 days, as well as those related to patient quality of life — loneliness, distress, uncontrolled pain, etc.
The transition from FFS to VBP is well underway with all 50 states moving forward with this model in 2022. All providers will want to hit the ground running with VBP and to ensure success, providers will need to look to the pilot states for lessons learned
during their implementation process so they can succeed.
Resources:
- Expanded HHVBP Model Frequently Asked Questions (PDF)
- HHVBP Model Composite Measure Calculation Steps (PDF)
- HHVBP Model Technical Specifications Composite Outcome Measures (PDF)
- HHVBP Model Newsletter April 2022 (PDF)
The AlayaCare Home Care Software Solution
AlayaCare is a fast-growing company that produces award-winning, cloud-based home healthcare software. With an end-to-end solution spanning clinical documentation, remote patient monitoring, client and family portals, mobile care worker functionality, APIs for system integration, a virtual care module, and more, we are uniquely suited to confront the challenges inherent to VBP.
As the only truly outcome-focused solution in the home care space today, AlayaCare not only offers the means to first collect and report on the data for payers, MCOs, and referral sources but allows home care providers to use AI tools to predict adverse events and see trends to intervene, if necessary, prior to seeing any failing VBP metrics.
As mentioned, this issue is complex, and many questions remain as to the best way forward. But one thing is certain: the best technology will help pave the way forward for the future success of VBP.
Sources
[1]. https://www.healthcatalyst.com/key-aco-and-value-based-purchasing-success-lowering-cost-structure
[4]. https://www.clinicient.com/blog/value-based-care-statistics/
[5]. https://revcycleintelligence.com/features/best-practices-for-value-based-purchasing-implementation


