Powering home-based care providers like who dare to deliver more
Power your agency and empower your team with our cloud-based solution.

Explore Solutions For:
Trusted by more than 700 customers and thousands of users around the world








Solutions for home-based care
Trusted by agencies across the care continuum
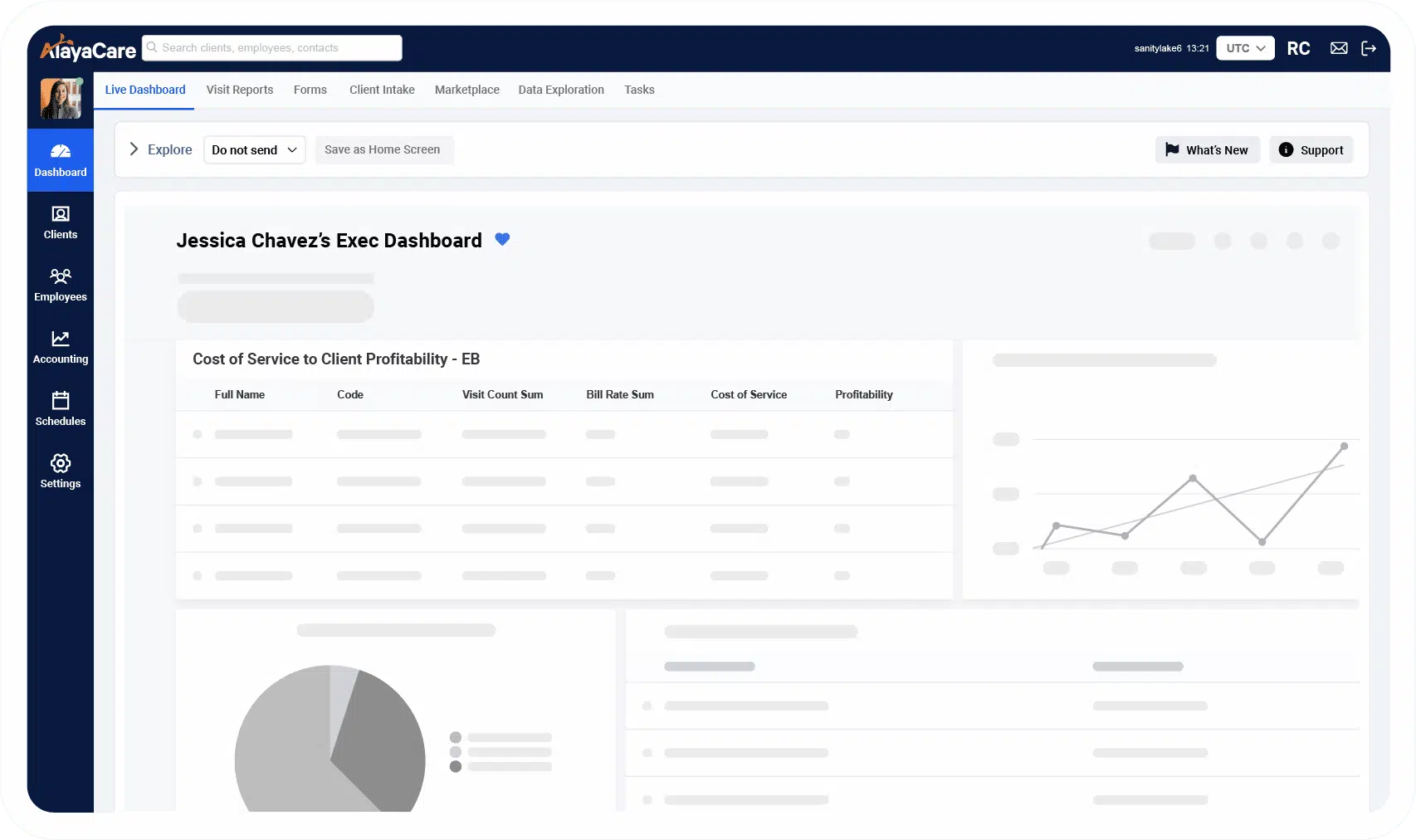
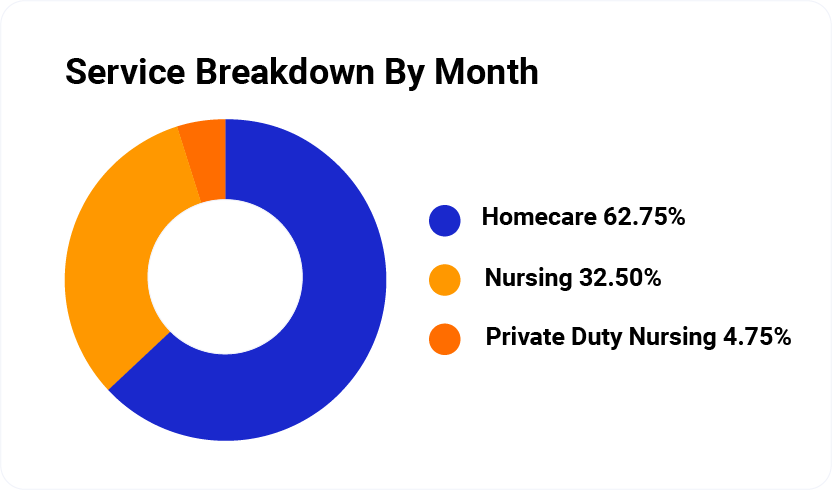
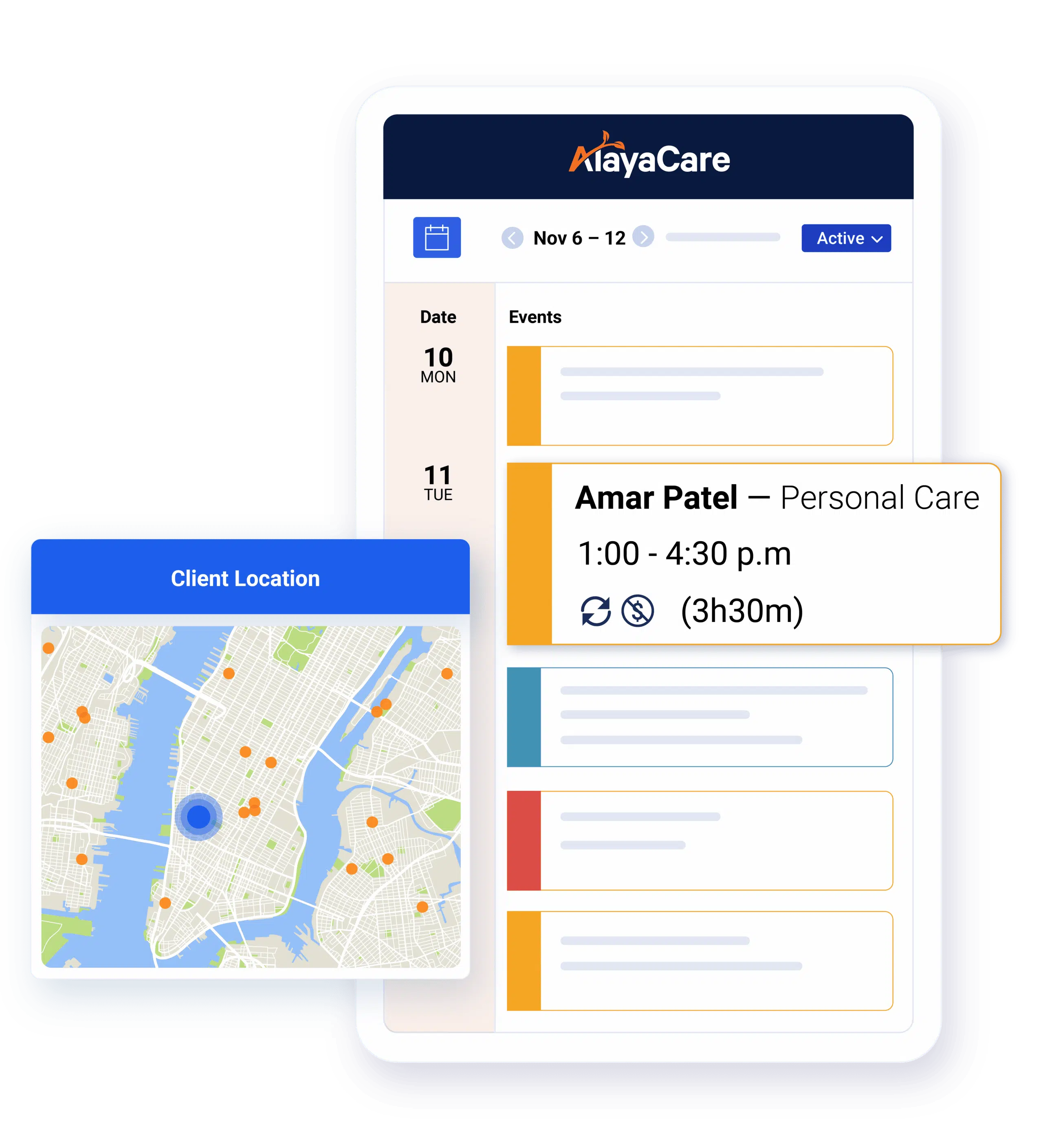
Efficient and effective home-based care relies on getting the details right. We put intake, scheduling, care management, billing, payroll, and all your data into a convenient desktop and mobile solution.
Home Care
Schedule staff, track performance, meet care plan goals and get data insights that make your decisions easier.
Learn MoreHome Health
Support all forms of care management, therapy and nursing needs wherever your client needs them.
Learn MoreInfusion
Stay on top of clinical documentation, optimize caregiver routing and scheduling and track care times.
Learn MoreHospice & Palliative Care
Keep hospice teams efficient, connected and focused on patient comfort and care.
Learn More
Why choose Alayacare
Better technology,
better outcomes
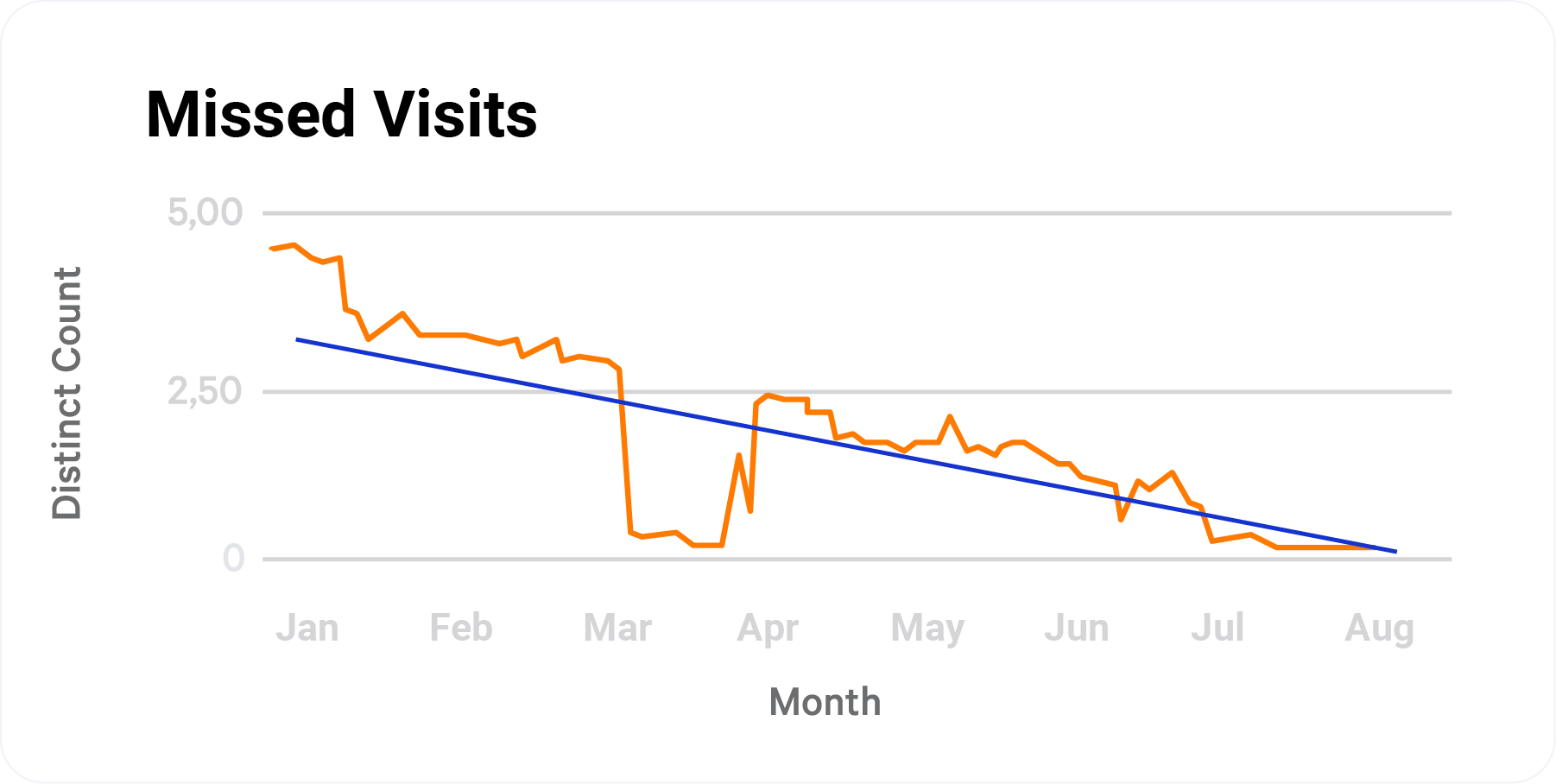
We make it possible to deliver the care of the future with modern, specialized solutions driven by data, insights and predictive AI, wherever your clients call home.
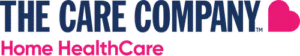
Empower your care providers with access to the clinical data, care plans and client details that create better client experiences.
Streamline time-consuming workflows, automate payroll with the help of custom reports, and keep your caregivers and office staff happy.
We make it possible for caregivers to do what they do best with the help of a platform that removes manual tasks and reduces errors.
AlayaCare by the numbers
Take a Tour
A closer look at AlayaCare
Choose a platform that will build your profit margin, mitigate business and compliance risk and that your caregivers enjoy using for a change. Choose AlayaCare.
Let's Talk
Ready to start? Book a demo and speak to an expert
See how AlayaCare can help your organization first-hand with a demo that will show you the benefits of our platform and answer all your questions.