The hospital-at-home model
Around the world, countries like the U.S., Canada, the U.K. and Australia are keying in on a new model of care in response to the growing need for modernized, adaptive care. This rising movement is toward hospital-at-home, a model in which health care providers can deliver hospital-level care in the comfort of a patient’s home.
The concept is rooted in the ongoing need to reduce patient load at hospitals, lower costs, prevent readmissions to hospital, and improve outcomes. Any time someone can avoid a trip to the hospital, or the clinic, and receive professional care or monitoring at home that keeps them safe – it is directly linked to better outcomes.
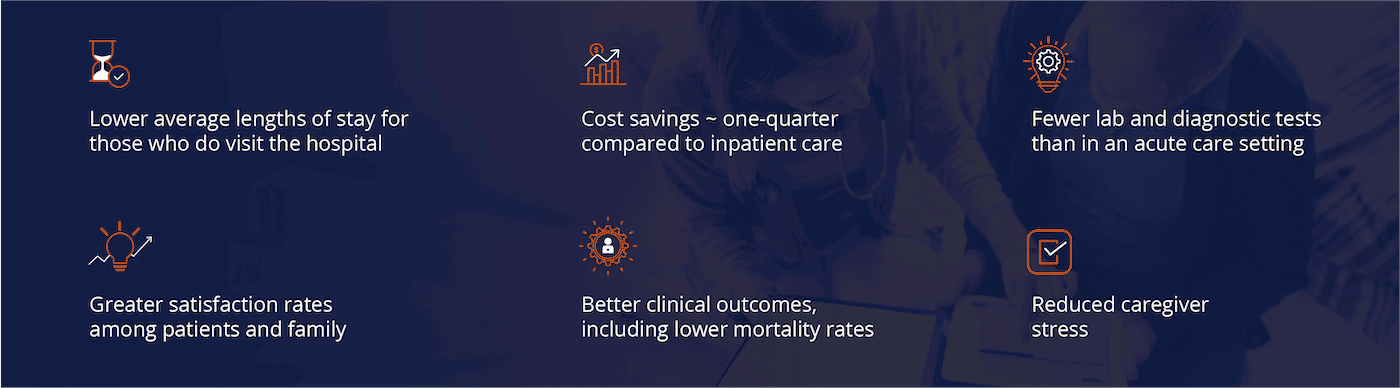
A hospital-at-home strategy leads to outcomes that favor patients and providers:
Not surprisingly, institutions across the world have been experimenting with how such a model could work for years now, as a potentially effective way to support patients whose care needs are not serious enough to warrant to trip to the hospital. In the U.S., the first to develop a hospital-at-home system was Johns Hopkins in the 1990s (a model validated in this 2005 study).
Official hospital-at-home program launches in U.S.
In November 2020, the U.S. Centers for Medicare & Medicaid Services (CMS) launched its Acute Hospital Care at Home effort as a method to reduce strain on hospitals caused by the COVID pandemic. This follows a Hospital Without Walls program from March 2020 that enabled hospitals to operate beyond their centers.
The newest program, built on a well of research confirming at-home care works, enables eligible hospitals to have the flexibility to treat certain patients in their homes. It is particularly beneficial for patients who would otherwise be admitted to hospital because they need to be monitored at least once a day for their ongoing care needs.
The program now counts 80 U.S. hospital systems... and growing.
More than 60 different acute conditions, such as asthma, congestive heart failure, pneumonia and COPD, can be treated appropriately and safely in home settings with proper monitoring and treatment protocols.
- CMS

The Rise of Hospital at Home
AlayaCare Blog Post
New Hospital-at-Home Waiver Program is 'Another Step Forward' for Home-Based Care
New CMS Hospital-at-Home Program Could Boost Business for Home Health Agencies
Requirements for the U.S. hospital-at-home program
What does this mean for home care providers?
The future of health care is in the home. Research has shown (like in this key U.S. study) that home-based non-urgent health care is as or more effective than in medical clinics. Home care agencies will be in the thick of the action: working with hospitals in regions they serve to provide home-based services. Hospital-at-home will work to serve people in their homes – but those people will soon want a long-term solution to staying well. And that is where home care organizations will come in.
And the fact is that many agencies are already able to shoulder the load. During the COVID crisis, many home health care organizations stepped up and instituted their own hospital-at-home programs by taking patients from local hospitals and setting them up with care plans at home. Many had to figure out the payer implications on the fly.
The fact is that home care agencies are set up to facilitate longer-term hospital-at-home plans. The opportunities are vast now that this model is being treated with the focus it very much deserves. Hospitals will be decompressed, and the home will be the environment of choice for everyone moving forward.
Knowing this escalating trend, agencies must ensure that their technological systems are flexible enough to enable this collaborative care. And it becomes now more important than ever to empower family caregivers with the training, knowledge and equipment to keep their loved ones safe. Home care agencies have the strongest lens on the family relationships and are key to enabling this important role.
Let's Talk
Ready to start? Book a demo and speak to an expert
See how AlayaCare can help your organization first-hand with a demo that will show you the benefits of our platform and answer all your questions.
